Community HealthChoices (CHC) is Pennsylvania’s new mandatory Medicaid managed care program. Pennsylvania is now using private managed care insurance companies (MCOs) to help improve the way the state provides medical care and services to the following groups:
- those enrolled in both Medicare and Medicaid (Medical Assistance)
- individuals on Medicaid waivers for physical disabilities and older adults
- Medicaid-eligible people who live in a nursing home
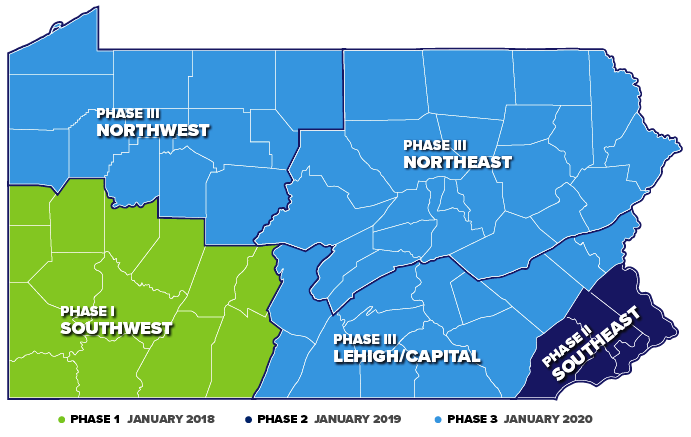
The state has rolled out Community HealthChoices in 3 phases in multi-county groupings. Phase 1 went into effect January 1, 2018. This includes the Southwestern part of the state including Allegheny County. This encompasses Pittsburgh along with 13 other surrounding counties. Phase 2 comprised the Southeast part of the state and took effect January 1, 2019. This included Philadelphia, Montgomery, Delaware, Chester and Bucks Counties. Finally, Phase 3 will see the rest of state join CHC on January 1, 2020. This includes the Northwest part of the state, the Northeast and the Lehigh/Capital Region.
How is it different from original Medicaid?
Community HealthChoices uses managed care insurance companies to administer Medicaid benefits. It will also replace the state’s Medicaid waiver programs for individuals age 21 and older and seniors who need long-term care. This means if you are Medicaid eligible, you will choose a health plan to manage all of your physical health care, and long-term services and supports. Instead of the ACCESS card, Medicaid benefits from the state will come through the CHC health plan that a subscriber picks.
According to HealthChoices.pa.gov CHC was developed to:
- enhance access to and improve coordination of medical care.
- create a person-driven, long-term support system. Therefore giving people more choice, control, and access to a full array of quality services that provide independence, health, and quality of life. Long-term services and supports help eligible individuals to perform daily activities in their home. Such activities include bathing, dressing, preparing meals, and monitoring of medications.
There are 3 CHC providers from which to choose:
What are the next steps?
For those in living in the Phase 3 region there is nothing you need to do at the moment. You do not need to apply for Community HealthChoices, because it is a mandatory program for people who qualify. The state Department of Human Services will send you information on how to enroll. Furthermore, be on the lookout for that information along with community education sessions in your local area. You can also eventually connect with an Independent Enrollment Broker, who can help you choose or change your plan. Call 1-844-824-3655 or visit EnrollCHC.com.
For a list of frequently asked questions (FAQs), visit EnrollCHC.com/getanswers.
Sources:
HealthChoices.pa.gov
Pennsylvania Health Access Network (PHAN)